In a world first international study led by Monash University researchers in Australia, the genetic markers for people with diabetes at risk of developing kidney disease have been identified.
The study opens the way for the development of a test that could predict those adults with Type 1 diabetes at risk of kidney disease before symptoms appear, allowing for doctors to introduce early-stage interventions.
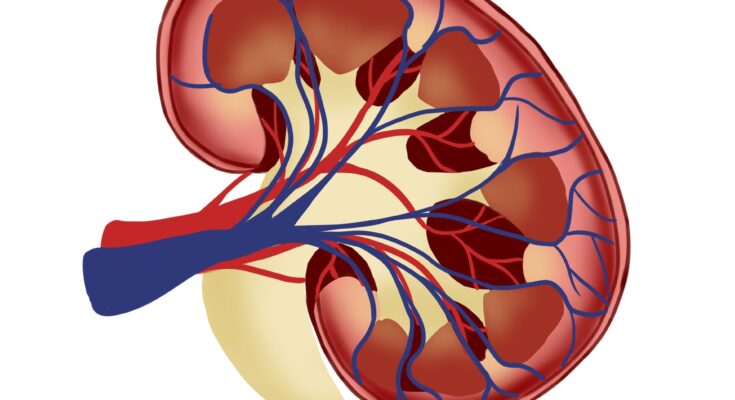
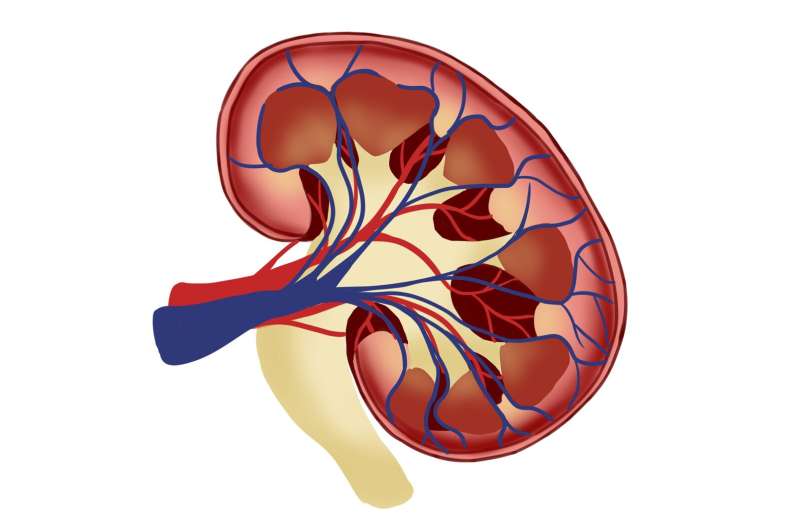
There are more than 500 million adults living with diabetes and approximately 1 in 4 adults will develop kidney disease. More than 80% of cases of end-stage renal disease are caused by diabetes which is also a risk for hypertension. The total number of people living with diabetes is projected to rise to 643 million by 2030 and 783 million by 2045.
The findings are from the largest-ever international study on type 1 diabetes, led by Professor Sam El-Osta, from Central Clinical School, Human Epigenetics team at the Department of Diabetes at Monash University and published in the Journal of Clinical Investigation.
The study tested the genes in 1017 Scandinavian and Asian diabetes cohorts, looking at the process called methylation, which is when a small molecule called a methyl group gets added to DNA. According to Professor El-Osta, the findings revealed “important clues that reduced DNA methylation is closely associated with the increased risk of diabetes relate kidney disease,” he said. “These discoveries will influence how we screen patients with diabetes and improve risk stratification, disease prediction and diagnosis.”
Currently standard assays used in the clinic rely on assessing kidney function and the level of damage to the kidney caused by diabetes—however the early stages of the disease are typically without symptoms. “We have developed a reliable method that improves predictive risk and diagnostic accuracy,” said the study’s first author Dr. Ishant Khurana, also from Monash University.
According to Professor El-Osta, despite the tremendous advances in genetic testing, no risk genes for diabetic kidney disease (DKD) have been identified. “The team at Monash University’s Central Clinical School using innovative sequencing techniques developed gene methylation risk scores that are tightly associated with early detection and the development of diabetic kidney disease,” he said.
“Scientists searching for blood-based biomarkers in diabetes cohorts originating from Finland, Denmark, Hong Kong and Thailand, found surprising commonality in gene methylation risk scores. They note that the innovative sequencing technologies developed using the internal collaboration revealed missing methylation data that was ultimately used to develop a predictive test for diabetic kidney disease.”
The researchers hope that routine gene methylation testing for diabetic complications such as kidney disease will soon be a standard part of the treatment plan, as it is for more common cancers.
“As far as technological advancements in methods are concerned, epigenetic testing is going to be the new standard for early detection and DKD care,” said Dr. El-Osta. “Renal biopsies are difficult to procure and the novel blood-based test means the test can be readily available and used in remote areas with the added advantage of being more stable than methods measuring other biological indices.”
This study was conducted by an international consortium comprising scientists at Monash University and collaborative partners in Helsinki, Copenhagen, Hong Kong and Bangkok.
More information:
Ishant Khurana et al, Reduced methylation corresponds with diabetic nephropathy risk in type 1 diabetes reduced methylation corresponds with diabetic nephropathy risk, Journal of Clinical Investigation (2023). DOI: 10.1172/JCI160959
Citation:
World first test to detect diabetics at risk of kidney disease (2023, January 18)
retrieved 19 January 2023
from https://medicalxpress.com/news/2023-01-world-diabetics-kidney-disease.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.
Source link