Diabetes is a huge and growing public health problem affecting millions of people in the U.S. It’s a disease in which patient self-management, supported by health information technology, can potentially prevent or reduce complications, improve quality of life and lower medical expenses.
There are more than 1,400 apps available for cell phones and tablets to help individuals living with diabetes manage their disease over the course of their lives, but use of these apps has been low. Getting diabetes patients who require insulin to continually use an app for support remains challenging. A new study from Regenstrief Institute, Indiana University Richard M. Fairbanks School of Public Health and Indiana University School of Medicine researchers explores diabetes patients’ perspectives on what they want from an app.
“To gain a better understanding of diabetes patients’ health behaviors and what they think is important for a diabetes app to do, we looked at patient motivation and studied views of app acceptability and usability as well as other factors that encourage use of these programs for successful disease self-management,” said Helen Fu, Ph.D., MSN, BSN, a postdoctoral public and population health informatics research fellow at Regenstrief Institute and IU Fairbanks School of Public Health, who led the study.
“We are especially interested in apps that are commercially available at no charge because these apps are accessible to the many underserved and low-income individuals living with diabetes.”
“Important questions that should be asked of all health apps, not just apps for diabetes, include, do they make the right calculations and do they make appropriate recommendations to patients?” said study co-author Regenstrief Institute Research Scientist Titus Schleyer, Ph.D., DMD.
“In this study we went beyond these basic questions and looked at how patients interact with apps and investigated factors that influence user success.” Dr. Schleyer co-directs the Regenstrief and Fairbanks School of Public Health Indiana Public and Population Health Informatics Fellowship program.
The 92 adult study participants had taken insulin for an average of 12 years. They reported a wide variety of diabetes complications including short-term memory loss, retinopathy and mobility impairment with the use of a cane, walker or wheelchair. The majority (70 percent) had type 2 diabetes.
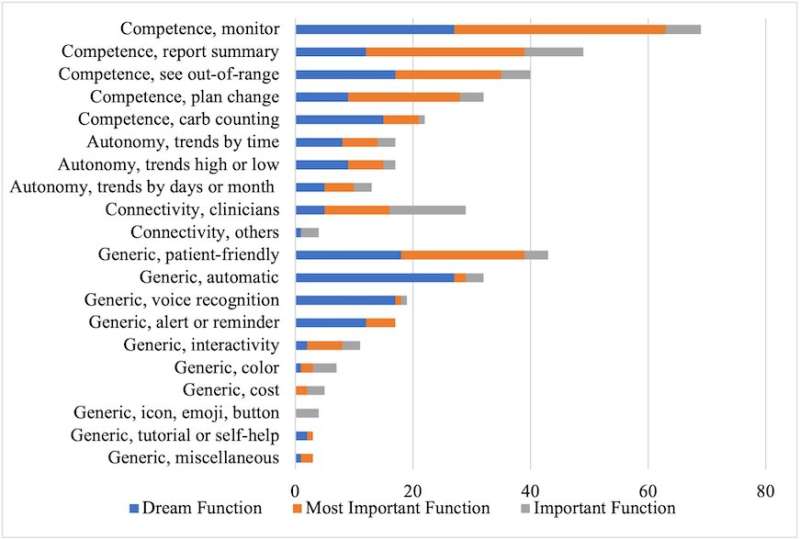
Most study participants wanted diabetes apps to save time regardless of functions, specifying that the app should be efficient and easy, requiring minimal user effort. Patient-friendly terminology and display and easy-to-understand reports were important to them as well.
Participants in the study said that a useful app could improve their sense of competence by helping them monitor data, create analysis reports and gain knowledge about reasons for blood glucose being out-of-range so they could plan behavior change. Some appreciated receiving information that guided them in adjusting their insulin dose.
Many said that apps improved their sense of autonomy when they showed if their blood glucose was trending high or low in relation to time of the day and day of the week.
Additionally, participants appreciated enhanced connectivity through which their clinicians could receive emails or print reports of home-monitored data via the app to better understand patients’ self-management behaviors.
“In a future study we plan to learn more about diabetes patients and ways to use health information technology to help them live more successfully with their disease,” said Dr. Fu. “We hope to find out which populations and subpopulations have the most trouble with disease management and to gain a better understanding of what well-designed tools might look like and share this information with clinicians and app developers.”
“There are many factors to consider—for example, older people may be unable to use the same apps as younger people—as we work toward long-term adoption of diabetes apps to support self-management by patients, as well as promote the integration of diabetes apps into the telehealth setting for clinicians,” said Dr. Schleyer.
The paper is published in the journal JMIR Diabetes.
More information:
Helen N C Fu et al, App Design Features Important for Diabetes Self-management as Determined by the Self-Determination Theory on Motivation: Content Analysis of Survey Responses From Adults Requiring Insulin Therapy, JMIR Diabetes (2022). DOI: 10.2196/38592
Citation:
What people want: Study explores patients’ perspectives on diabetes self-management apps (2023, June 1)
retrieved 1 June 2023
from https://medicalxpress.com/news/2023-06-people-explores-patients-perspectives-diabetes.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.
Source link




