In a study recently published in the Journal of Clinical Investigation, researchers at Juntendo University investigate a biomolecule that mitigates eczema in mice
Atopic dermatitis (AD), more colloquially known as eczema, is an inflammatory condition that manifests as itchy rashes on the skin. The disease flares up periodically over a patient’s lifetime causing mild to severe discomfort. What’s more, the treatment for refractory AD remains unsatisfactory. Now, a team of researchers from Juntendo University, led by François Niyonsaba, has revealed a candidate called human-β-defensin-3 (hBD-3) with potential in this regard.
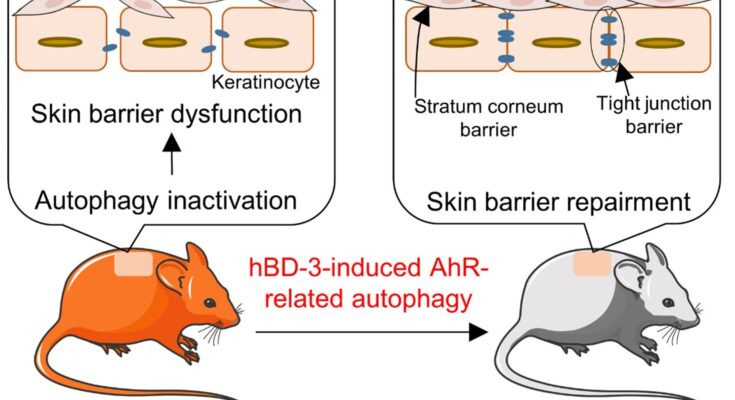
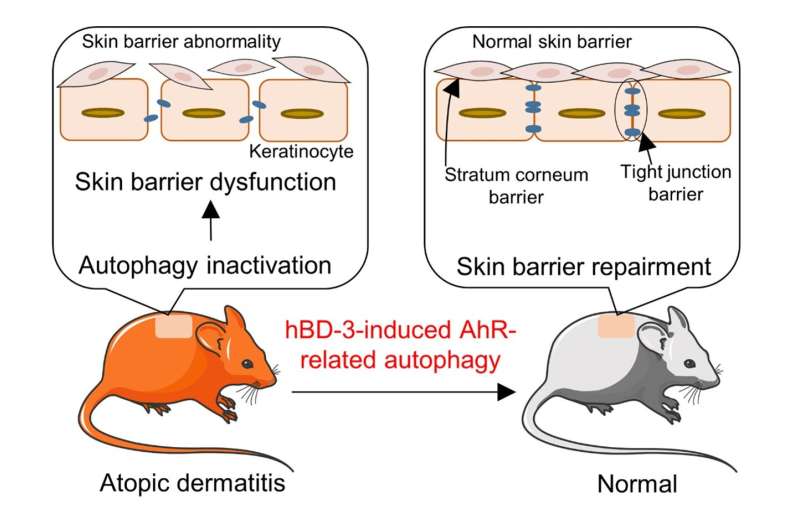
One of the characteristics of AD is the disruption of the outermost layer of the skin: the epidermal barrier. Inside the cells that line this barrier, a mechanism called autophagy is involved in their differentiation and antimicrobial activity. Autophagy is a process by which damaged cells are degraded. Linking these two phenomena, the team started off by scrutinizing the association between autophagy and skin barrier function in AD and then proceeded to investigate hBD-3, a regulator of autophagy, in combating the condition.
Using the skin of human patients and mice with AD, the state of autophagy in affected cells was first analyzed. Molecules that typically drive autophagy and autophagic structures were reduced, suggesting that autophagy was indeed inhibited in these cells. When skin cells were examined closely to understand why autophagy was diminished, a class of molecules known as interleukins (which are typically released by our immune system) emerged as the culprits. Next, the role of autophagy in maintaining a healthy skin barrier was assessed by mutating mice to remove all programming for autophagy in the skin. These mice produced less proteins that are essential for developing a skin barrier. They were more susceptible to developing inflammation and lesions on their skin, similar to AD.
hBDs are biomolecules that have shown promise in restoring epidermal barrier function. Thus, the next focus was on understanding whether they play a role in restoring barrier function by regulating autophagy. Of the four types of hBDs found in human skin, one subtype, hBD-3, successfully increased autophagy in skin cells, which subsequently resulted in the development of skin barrier proteins. hBD-3 did so by activating the aryl hydrocarbon receptor (AhR) signaling—a cellular pathway responsible for proper barrier function. The researchers also confirmed this hypothesis in mice. When mice with AD were administered mBD-14 (the mouse analog of hBD-3) they showed marked improvement in inflammation. However, this inflammation improvement was not observed in mice with a deficiency in skin autophagy or inhibition of AhR, highlighting the importance of autophagy and AhR as the mechanism of mBD-14/hBD-3 action.
“Thus, autophagy contributes to the pathogenesis of AD, and hBD-3 could be used for therapeutic purposes,” concludes Niyonsaba’s research group. This study gives dermatologists deeper insights into autophagy as a driving force behind AD and a possible solution to overcome it.
Ge Peng et al, Human β-defensin-3 attenuates atopic dermatitis–like inflammation through autophagy activation and the aryl hydrocarbon receptor signaling pathway, Journal of Clinical Investigation (2022). DOI: 10.1172/JCI156501
Provided by
Juntendo University
Citation:
Researchers investigate a biomolecule that mitigates eczema in mice (2022, September 29)
retrieved 29 September 2022
from https://medicalxpress.com/news/2022-09-biomolecule-mitigates-eczema-mice.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.
Source link